Guided Bone Regeneration (GBR) and Guided Tissue Regeneration (GTR) are biological approaches to regenerate lost bone and tissue. These techniques are crucial for treating defects caused by disease or injury.
Overview of Guided Bone Regeneration (GBR) and Guided Tissue Regeneration (GTR)
GBR and GTR use barrier membranes to guide cellular growth, preventing soft tissue invasion and promoting osseous regeneration. They are widely applied in dental and orthopedic surgeries.
Importance of Bone and Tissue Regeneration in Dental and Orthopedic Applications
These techniques are vital for enhancing bone growth in implant placements and repairing tissue defects. They revolutionized treatments, offering predictable outcomes and improving patient recovery rates significantly.
Guided Bone Regeneration (GBR) and Guided Tissue Regeneration (GTR) are surgical techniques that utilize barrier membranes to guide cellular growth. GBR focuses on enhancing bone formation, often combined with bone grafts, while GTR targets periodontal tissue repair. These methods prevent soft tissue migration into defect sites, allowing bone cells to regenerate effectively. They are widely applied in dental and orthopedic surgeries to address defects caused by disease or injury. The success of these procedures relies on the precise placement of membranes to ensure proper tissue regeneration and long-term functional recovery.
Bone and tissue regeneration are crucial for restoring function and aesthetics in dental and orthopedic cases. In dentistry, these techniques enable successful implant placement by addressing bone loss, while in orthopedics, they repair defects from injuries or degenerative conditions. Regeneration prevents further tissue deterioration, enhances patient recovery, and improves quality of life. Advanced biomaterials and barrier membranes play a key role in promoting predictable outcomes. These methods are integral to modern reconstructive surgeries, offering reliable solutions for complex bone and tissue defects, making them indispensable in both fields.
History and Evolution of Guided Bone and Tissue Regeneration
Guided bone regeneration emerged in the 1980s, evolving from early concepts of barrier membranes to modern techniques. Key milestones include advancements in membrane technology and biomaterials.
Early Developments in GBR and GTR Techniques
Guided bone regeneration (GBR) and guided tissue regeneration (GTR) emerged in the 1980s, with early techniques focusing on barrier membranes to prevent soft tissue migration. Initial membranes were non-resorbable, but later resorbable materials were developed. The concept of GBR was first explored by Dahlin and Nygaard in 1988, using millipore filters in animal models. These early studies demonstrated the potential for osseous regeneration. The introduction of collagen membranes marked a significant advancement, improving biocompatibility and clinical outcomes. These foundational developments laid the groundwork for modern regenerative therapies, enabling predictable bone and tissue growth in dental and orthopedic applications.
Key Milestones in the Advancement of Regenerative Therapies
Significant advancements include the development of bioactive glass for bone regeneration and the introduction of platelet-rich fibrin (PRF) membranes. These innovations enhanced predictability and biocompatibility. The integration of nanotechnology improved membrane properties, while stem cell therapies offered new possibilities. These milestones have refined GBR and GTR techniques, enabling more effective tissue repair and bone growth. Such progress underscores the evolving nature of regenerative therapies, paving the way for advanced treatments in dental and orthopedic applications.
Fundamental Principles of Guided Bone and Tissue Regeneration
Guided regeneration relies on barrier membranes to prevent soft tissue migration, allowing bone and tissue cells to populate defect sites. Bone grafts or substitutes provide structural support.
Hypoxia plays a critical role in modulating regenerative processes, influencing cellular activity and tissue repair. These principles ensure targeted healing and minimize complications in surgical procedures.
Biological Mechanisms Behind Bone and Tissue Regeneration
Bone and tissue regeneration involves complex biological processes, including cell migration, differentiation, and angiogenesis. Progenitor cells, such as osteoblasts and fibroblasts, play a central role in repairing defects. Hypoxia, a key regulator, enhances regenerative potential by stimulating angiogenesis and promoting the release of growth factors. These factors, such as BMPs and PDGF, orchestrate cellular activity, ensuring targeted tissue repair. The process is further supported by biomaterials, like bioactive glass, which mimic natural bone structures, fostering an environment conducive to regeneration. Understanding these mechanisms is crucial for optimizing GBR and GTR outcomes, enabling precise guidance of bone and tissue healing.
Role of Barrier Membranes in Preventing Soft Tissue Migration
Barrier membranes are critical in guided regeneration, preventing soft tissue invasion into bone defects. These membranes create a protective environment, allowing osteogenic cells to populate the defect. Non-collagen and collagen membranes differ in biocompatibility and biodegradation, with collagen membranes often showing superior tissue integration. Their structure and material properties ensure minimal tissue interference while promoting bone growth. The swelling index and degradation rates of these membranes are key factors in their effectiveness, ensuring proper tissue guidance during the healing process. This separation of soft and hard tissues is essential for successful osseous regeneration in both dental and orthopedic applications.
Importance of Hypoxia in Regenerative Processes
Hypoxia plays a critical role in regenerative processes by modulating cellular responses. Low oxygen levels can enhance the expression of growth factors and promote angiogenesis, essential for tissue repair. However, excessive hypoxia can impede regeneration by slowing cellular activity. In guided bone and tissue regeneration, hypoxia influences osteoblast and stem cell behavior, affecting bone formation. Managing oxygen levels is crucial for optimizing regenerative outcomes, as it balances the need for cellular activation and prevention of tissue hypoxia-induced complications. Understanding hypoxia’s dual role is key to advancing therapeutic strategies in dental and orthopedic applications.

Applications of Guided Bone and Tissue Regeneration
Guided bone and tissue regeneration is widely applied in dental implantology, orthopedics, and periodontal treatments. It enhances bone growth for implants, repairs defects, and restores tissue integrity.
Dental Applications: Enhancing Bone Growth for Implant Placement
In dental implantology, guided bone regeneration (GBR) is essential for patients with insufficient bone density. Barrier membranes and bone grafts are used to create a conducive environment for osseous healing, ensuring implant stability and aesthetics. This technique prevents soft tissue migration, allowing bone cells to regenerate effectively. Successful outcomes enable long-term implant functionality and patient satisfaction, making GBR a cornerstone in modern dental reconstructive procedures.
Orthopedic Applications: Treating Bone Defects and Injuries
Guided bone regeneration (GBR) is a vital technique in orthopedics for addressing bone defects and injuries. By employing barrier membranes and bone grafts, GBR promotes osseous healing, preventing soft tissue encroachment. This method is particularly effective in treating large bone defects, fractures, and non-union cases. The use of bioactive materials enhances regeneration, fostering a conducive environment for natural bone repair. Advances in membrane technology and the integration of growth factors further improve outcomes, making GBR a cornerstone in orthopedic treatments aimed at restoring structural integrity and functional mobility in patients with complex bone injuries.
Periodontal Applications: Regenerating Lost Periodontal Tissue
Guided tissue regeneration (GTR) is instrumental in periodontal therapy, focusing on the regeneration of lost periodontal tissue and supporting bone. This technique uses barrier membranes to prevent gingival tissue ingress, allowing periodontal ligament cells to repopulate the defect. GTR is particularly effective in treating deep pockets and furcation defects, halting disease progression and restoring tooth support. Clinical studies highlight its predictability, with significant improvements in pocket depth and attachment levels. The integration of bioactive materials and growth factors further enhances outcomes, offering a reliable solution for patients with advanced periodontal disease, thereby extending tooth longevity and improving oral health.

Barrier Membranes in Guided Bone and Tissue Regeneration
Barrier membranes are critical for guiding cellular growth, preventing soft tissue migration, and promoting osseous regeneration. Their design focuses on biocompatibility, durability, and controlled biodegradation to optimize healing outcomes.
Types of Membranes: Non-Collagen vs. Collagen Membranes
Barrier membranes are categorized into non-collagen and collagen types. Non-collagen membranes, often synthetic (e.g., PTFE or titanium), are durable and resistant to collapse, making them ideal for long-term use. They can be resorbable or non-resorbable, depending on material and application. Collagen membranes, derived from natural sources, are biocompatible and promote tissue integration, with controlled resorption rates. Non-collagen membranes are preferred for structural support, while collagen membranes enhance tissue regeneration due to their ability to attract cells and integrate seamlessly with host tissue, offering distinct advantages in guided bone and tissue regeneration procedures.
Comparative Characteristics of Different Membrane Materials
Membrane materials vary in biocompatibility, resorbability, and mechanical strength. Collagen membranes are biodegradable and promote tissue integration, with controlled resorption rates, making them ideal for healing. Non-collagen membranes, such as PTFE or titanium, are non-resorbable and offer long-term structural support. Synthetic membranes like polymer-based materials provide durability and resistance to collapse. Each material has distinct advantages: collagen membranes enhance tissue regeneration, while non-collagen membranes ensure stability. Selection depends on defect type, healing goals, and patient needs, with collagen membranes often favored for their biological compatibility and non-collagen for structural integrity in guided bone and tissue regeneration procedures.
Swelling Index and Biodegradation Rates of Membranes
The swelling index and biodegradation rates of membranes significantly influence their effectiveness in guided bone and tissue regeneration. Membranes with higher swelling indices maintain space more effectively, preventing soft tissue migration. Collagen membranes exhibit controlled resorption, aligning with tissue healing timelines, while non-collagen membranes, like PTFE, remain stable longer but may require removal. Biodegradation rates must balance tissue integration and structural support to avoid premature membrane breakdown or prolonged foreign body reactions. These characteristics are critical in selecting membranes for specific clinical applications, ensuring optimal regeneration outcomes and minimizing complications in both bone and tissue repair processes.

Bone Grafts and Substitutes in Guided Bone Regeneration
Bone grafts and substitutes are essential for promoting osseous regeneration. Autografts, allografts, and xenografts are commonly used, while bioactive glass and other substitutes enhance bone healing in GBR.
Types of Bone Grafts: Autografts, Allografts, and Xenografts
Bone grafts are classified into autografts, allografts, and xenografts. Autografts, taken from the patient’s own body, offer high biocompatibility and osteogenic potential. Allografts, derived from donors, are a viable alternative when autografts are limited. Xenografts, sourced from animals, are processed to ensure safety and compatibility. Each type has unique advantages, with autografts being the gold standard due to their ability to promote rapid healing and integration. These grafts are widely used in GBR to fill defects, enhance bone density, and support implant placement, ensuring optimal regenerative outcomes in dental and orthopedic procedures.
Role of Bone Substitutes in Promoting Osseous Regeneration
Bone substitutes play a pivotal role in osseous regeneration by providing a scaffold for bone growth. These materials, such as bioactive glass and synthetic ceramics, mimic natural bone structure, enhancing cell attachment and proliferation. They are biocompatible and resorbable, gradually integrating with host tissue. Bone substitutes reduce reliance on autografts, minimizing donor site morbidity. Their porosity and surface properties promote vascularization and osteogenesis, making them indispensable in GBR. By filling bone defects and stabilizing grafts, substitutes ensure predictable outcomes, fostering successful bone regeneration in dental and orthopedic surgeries.
Particulate Bioactive Glass as a Promising Material
Particulate bioactive glass emerges as a highly effective material in guided bone regeneration. Its unique composition promotes osteogenesis by stimulating osteoblast activity and enhancing bone matrix formation. The material’s high surface area and porosity facilitate cell attachment and proliferation. Bioactive glass is resorbable, gradually dissolving as new bone forms, and promotes vascularization, which is critical for tissue repair. Its ability to integrate seamlessly with host tissue makes it an excellent choice for treating bone defects. This material is particularly advantageous in dental applications, offering a reliable solution for achieving predictable bone regeneration outcomes.

Recent Innovations in Guided Bone and Tissue Regeneration
Recent advancements include improved membrane biocompatibility and the integration of growth factors and stem cells, enhancing regenerative outcomes and reducing recovery times significantly.
Advancements in Membrane Technology and Biocompatibility
Recent innovations in membrane technology have focused on enhancing biocompatibility and performance. Non-collagen and collagen membranes now offer improved swelling indexes and controlled biodegradation rates, optimizing tissue regeneration.
Studies highlight domestic membrane development with in vitro assessments, ensuring reliable biodegradation and compatibility. These advancements reduce complications and improve surgical outcomes, making membranes more effective in guided regeneration procedures.
Use of Platelet-Rich Fibrin (PRF) Membranes
Platelet-rich fibrin (PRF) membranes are increasingly used in guided bone and tissue regeneration due to their biocompatibility and ability to enhance healing. Derived from the patient’s blood, PRF is rich in growth factors that stimulate cellular activity and tissue repair.
Studies demonstrate PRF’s effectiveness in promoting bone regeneration, particularly in cases with insufficient alveolar ridge width. Its autologous nature reduces immune reactions, making it a safer and more efficient option for surgical procedures. PRF membranes also support faster recovery and are cost-effective, offering promising results in both dental and orthopedic applications.
Incorporation of Growth Factors and Stem Cell Therapies
Growth factors, such as bone morphogenetic proteins (BMP-2) and transforming growth factor-beta (TGF-β), play a pivotal role in enhancing bone and tissue regeneration. These proteins stimulate cellular proliferation, differentiation, and extracellular matrix deposition, accelerating the healing process.
Stem cell therapies, particularly mesenchymal stem cells (MSCs), are being integrated into regenerative protocols. MSCs can differentiate into osteoblasts, promoting bone formation. Combining growth factors with stem cells and biocompatible scaffolds further enhances osteoconductivity, offering innovative solutions for complex defects and improving surgical outcomes.

Clinical Practices and Surgical Techniques
Clinical practices involve precise surgical techniques using barrier membranes and bone grafts to regenerate bone and tissue. These methods ensure predictable outcomes in dental and orthopedic surgeries.
Surgical Procedures for Guided Bone and Tissue Regeneration
Surgical procedures involve creating an incision, placing a barrier membrane, and securing it with bone grafts or bioactive materials. The membrane prevents soft tissue migration, allowing bone cells to regenerate.
The procedure ensures proper healing by maintaining space for bone growth. Postoperative care is critical to prevent complications and promote successful tissue regeneration.
Case Studies: Successful Outcomes and Challenges
Case studies highlight the effectiveness of guided bone and tissue regeneration in treating bone defects. For instance, bioactive glass implants in rabbits showed significant bone repair within 12 weeks.
Platelet-rich fibrin (PRF) membranes demonstrated successful tissue regeneration in patients with insufficient alveolar ridge width.
However, challenges such as membrane degradation and incomplete regeneration have been reported. These studies emphasize the need for precise surgical techniques and patient-specific approaches to optimize outcomes.
Postoperative Care and Patient Management
Proper postoperative care is essential for successful outcomes in guided bone and tissue regeneration. Patients should maintain good oral hygiene, avoiding trauma to the surgical site.
Pain management and anti-inflammatory medications are often prescribed to ensure comfort and minimize swelling. Regular follow-ups are crucial to monitor healing progress and address any complications early.
Smoking and strenuous activities should be avoided to promote optimal healing. Aseptic techniques and patient adherence to postoperative instructions significantly influence the success of regenerative procedures and tissue integration.

Evaluation and Monitoring of Regenerative Outcomes
Evaluation involves imaging techniques like X-rays and CT scans to assess bone growth. Histological assessments using hematoxylin-eosin staining provide detailed tissue repair insights. Long-term monitoring ensures sustained regeneration success.
Imaging Techniques: X-ray and CT Scan Analysis
X-rays and CT scans are essential tools for monitoring regenerative outcomes. X-rays provide initial assessments of bone density and growth, while CT scans offer detailed 3D imaging of tissue repair. These techniques allow clinicians to track progress over time, such as at 2, 4, 8, and 12 weeks post-implantation. Imaging helps verify the integration of bioactive materials and the formation of new bone tissue. Regular analysis ensures accurate evaluations of regeneration success, guiding clinical decision-making and confirming the efficacy of guided bone and tissue regeneration procedures in both dental and orthopedic applications.
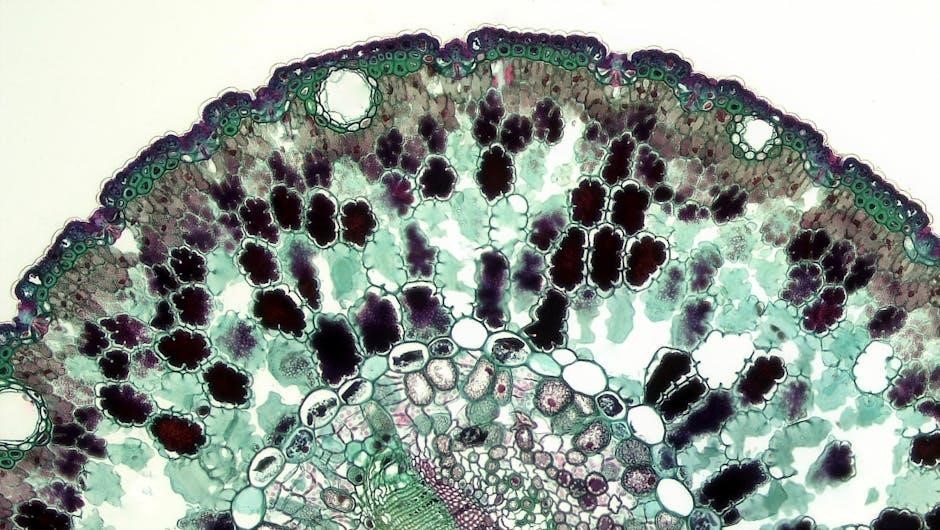
Histological Assessment Using Hematoxylin-Eosin Staining
Histological assessment with hematoxylin-eosin (H&E) staining is a critical method for evaluating tissue repair and regeneration. This technique involves staining tissue samples to visualize cellular structures and assess the extent of bone and tissue healing. In studies, H&E staining has been used to observe tissue repair in bone defect regions at 2, 4, 8, and 12 weeks post-implantation. The staining helps identify newly formed bone, collagen deposition, and cellular infiltration, providing detailed insights into the regenerative process. This method complements imaging techniques like X-rays and CT scans, offering a microscopic view of tissue composition and confirming the success of guided bone and tissue regeneration.
Long-Term Follow-Up and Success Rates
Long-term follow-up is essential to evaluate the durability and success of guided bone and tissue regeneration. Studies demonstrate that these techniques yield high success rates, with noticeable bone growth and tissue repair observed over time. Imaging techniques like X-rays and CT scans are used to monitor bone density and volume, while histological assessments confirm tissue composition. Success rates are influenced by factors such as membrane biocompatibility, patient health, and surgical precision. With advancements in materials and methods, long-term outcomes continue to improve, offering reliable solutions for patients requiring bone and tissue reconstruction.

Challenges and Limitations in Guided Bone and Tissue Regeneration
Key challenges include membrane degradation, hypoxia, and variability in patient response. These factors can hinder regeneration efficiency and lead to complications, impacting overall success rates.
Factors Influencing the Success of Regenerative Procedures
The success of guided bone and tissue regeneration depends on multiple factors, including patient-specific biological responses, such as healing capacity and vascular supply. The type and quality of barrier membranes, bone graft materials, and their biocompatibility play a critical role. Surgical technique and operator expertise are equally important, as improper membrane placement or instability can lead to complications; Additionally, postoperative care, including infection control and patient compliance, significantly impacts outcomes. The severity and location of the defect, as well as systemic health conditions, also influence the efficacy of regenerative procedures. These factors collectively determine the predictability and success of GBR and GTR.
Complications Arising from Membrane Degradation
Membrane degradation is a critical factor affecting the outcome of guided bone and tissue regeneration. Premature degradation can lead to incomplete bone formation and soft tissue invasion, compromising the procedure. Hypoxia, a common issue, slows regenerative processes, including membrane degradation, potentially reducing the efficacy of GBR and GTR. Additionally, poor biocompatibility or improper membrane fixation can cause inflammation or infection, further complicating healing. The chronic nature of infections and lack of keratinized tissue also exacerbate these issues. Addressing these challenges requires careful material selection and surgical precision to ensure predictable and successful regenerative outcomes, as highlighted in recent studies by AG Stepanov and others.
Impact of Hypoxia on Regenerative Processes
Hypoxia significantly influences bone and tissue regeneration, slowing down regenerative processes. It affects cellular activities, including proliferation and differentiation, critical for osseous wound healing. While acute hypoxia can stimulate angiogenesis, chronic hypoxia impairs regeneration by disrupting the balance of oxygen levels and growth factor expression. This duality highlights the complexity of managing hypoxia in guided bone and tissue regeneration. Studies by Dahlin et al. and others emphasize the need to address hypoxia for optimal outcomes, ensuring predictable results in both dental and orthopedic applications.

Future Perspectives and Research Directions
Emerging biomaterials and nanotechnology are revolutionizing guided bone and tissue regeneration. Advances in membrane technology, growth factors, and stem cell therapies promise enhanced regenerative outcomes and minimized complications.
Emerging Biomaterials for Enhanced Regeneration
Recent advancements in biomaterials, such as bioactive glass and nanocomposite scaffolds, are transforming guided bone and tissue regeneration. These materials mimic natural bone structure, promoting cellular attachment and proliferation. Bioactive glass, for instance, stimulates osteogenesis through ionic interactions, while nanotechnology enhances scaffold porosity and mechanical strength. Composite materials combining collagen and synthetic polymers are also being explored for their biocompatibility and biodegradability. These innovations aim to create customizable, patient-specific solutions for bone and tissue defects, offering improved regeneration outcomes and faster recovery times. In vivo studies demonstrate their potential in enhancing osseous repair and integration.
Role of Nanotechnology in Tissue Engineering
Nanotechnology is revolutionizing tissue engineering by creating nanostructured scaffolds that mimic the extracellular matrix. These scaffolds enhance cellular activities like proliferation and differentiation, crucial for bone and tissue regeneration. Nanocomposite materials combine natural and synthetic components, improving biocompatibility and biodegradability. Nanoparticles can deliver growth factors precisely, promoting targeted regeneration. In vivo studies demonstrate that nanotechnology improves scaffold mechanical properties and biological interactions, leading to better bone defect repair. These advancements enable tailored, patient-specific solutions, enhancing the predictability and success of regenerative therapies in dental and orthopedic applications. Nanotechnology’s potential in tissue engineering continues to expand, offering innovative solutions for complex defects.
Potential of Bioactive Scaffolds in Bone Regeneration
Bioactive scaffolds play a pivotal role in bone regeneration by providing a three-dimensional framework that promotes cellular attachment, proliferation, and differentiation. These scaffolds are designed to mimic the natural extracellular matrix, enhancing osteoconductivity and osteoinductivity. By incorporating bioactive materials, such as hydroxyapatite and bioactive glass, scaffolds can stimulate bone formation and improve integration with host tissue. Additionally, bioactive scaffolds can deliver growth factors and therapeutic agents, further enhancing regenerative outcomes. Their biocompatibility and biodegradability make them ideal for promoting bone healing in defects. This innovative approach holds significant potential for advancing bone regeneration therapies in both dental and orthopedic applications.
Guided bone and tissue regeneration, through GBR and GTR, significantly enhances dental and orthopedic outcomes, offering predictable bone growth and tissue repair, with promising future advancements in regenerative therapies.
Guided bone and tissue regeneration (GBR and GTR) are biological techniques that use barrier membranes to direct cellular growth, preventing soft tissue infiltration and promoting osseous repair. These methods are essential in dental and orthopedic surgeries to address defects caused by disease or injury. The success of these procedures depends on membrane type, biodegradation rates, and the use of bone grafts or substitutes. Recent advancements, such as bioactive materials and growth factors, have enhanced predictability and outcomes. These therapies hold significant promise for future innovations in regenerative medicine, offering improved patient recovery and tissue reconstruction.
Impact on Modern Dental and Orthopedic Practices
Guided bone and tissue regeneration has revolutionized dental and orthopedic treatments, offering reliable solutions for bone defects and tissue loss. These techniques enhance implant placement success rates and improve patient outcomes. The use of advanced biomaterials and barrier membranes has minimized complications, enabling less invasive procedures. GBR and GTR have become cornerstone therapies, setting new standards in regenerative medicine. Their integration into modern practices has significantly improved the predictability of surgical outcomes, addressing complex cases with precision and efficiency. This has transformed patient care, making it more effective and accessible for a wide range of clinical scenarios.
Promise of Future Advances in Regenerative Therapies
Promises of Future Advances in Regenerative Therapies
Future advancements in guided bone and tissue regeneration hold immense potential, driven by emerging biomaterials and technologies. Nanotechnology and bioactive scaffolds are expected to enhance regeneration efficiency, while stem cell therapies and growth factors may further optimize outcomes. Innovations in membrane design and biodegradable materials promise improved biocompatibility and predictability. These developments could lead to more personalized treatments, reducing recovery times and improving patient satisfaction. The integration of advanced imaging and monitoring tools will also play a crucial role in refining procedures. As research progresses, these therapies are likely to become more accessible and effective, transforming the landscape of regenerative medicine.

